Abstract
Introduction:
BK virus associated hemorrhagic cystitis (BK-HC) is a common complication after allogeneic hematopoietic stem cell transplantation (allo-HCT), with incidence up to 70%. BK virus is a widely prevalent non-encapsulated DNA human polyomavirus which latently infects the uroepithelium and reactivates during immunosuppression. While its pathogenesis is not yet clearly elucidated, BK-HC is associated with factors related to transplant procedure (myeloablative conditioning regimen), graft source (unrelated donor, HLA mismatching), onset of acute graft-versus-host disease, and high-level urinary BK viral replication. Symptomatic and supportive measures have been the standard of care for many years for this difficult-to-treat complication. Treatments that have been trialed include antivirals, antibiotics, and immunomodulatory agents. Cidofovir is a nucleotide analog of cytosine that is active against various DNA viruses with growing evidence as a therapeutic option for BK-HC. The aim of the present retrospective study is to assess the safety profile and efficacy of intravenous and intravesical cidofovir in allo-HCT patients with BK-HC.
Methods:
We conducted a retrospective study of the allo-HCT patient cohort from January 2010 until March 2017 in a single center in Ontario, Canada. All patients who underwent allo-HCT and received cidofovir for symptomatic BK-HC (hematuria with BK viruria and/or viremia) were included. Electronic charts were reviewed for patient characteristics, cidofovir prescription data, clinical outcomes, and toxicities. BK-HC severity was graded as: Grade 1 (microscopic hematuria), Grade 2 (macroscopic hematuria), Grade 3 (macroscopic hematuria with clots), Grade 4 (impaired renal function). Clinically efficacy was assessed at the end of cidofovir treatment as: Complete Response (CR) - complete symptom remission, Partial Response (PR) - downgrading of severity, or No Response - unchanged or worsening severity. The primary outcome was response to cidofovir, as defined by PR or CR. Secondary outcomes include overall survival, BK virus levels (both urine and blood), and renal toxicity (increase Cr > 30 µmol/L).
Results:
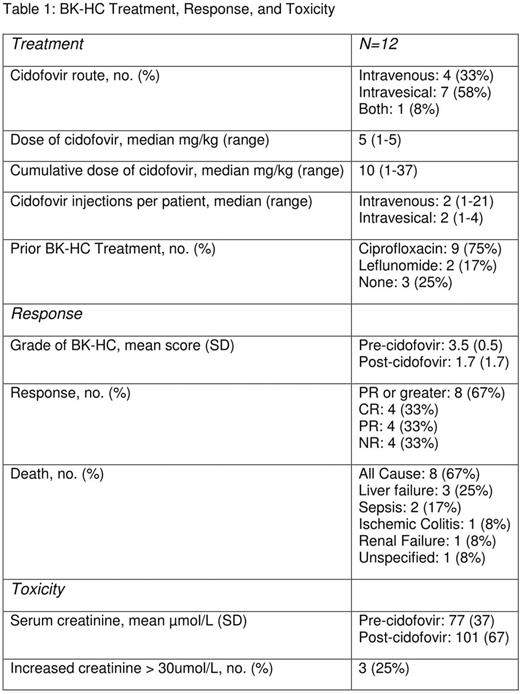
Twelve allo-HCT patients (6 male, 6 female; median age 49) with BK-HC were treated with cidofovir at our center. The majority of transplants were from 10/10 HLA matched related donors and complicated by acute GVHD and CMV viremia. Median time to BK-HC was 82 days (23-762 days), with an initial clinical grade of 3 (50%) or 4 (50%). All patients had BK viruria, whereas 2 did not have BK viremia. Prior therapies were received by most patients, specifically ciprofloxacin (75%) or leflunomide (17%). Cidofovir administration was via intravenous (33%), intravesical (58%), or both modalities (8%). Median cumulative dose was 10 mg/kg (1-37 mg/kg) across a median of 2 doses (1-21 doses) with a median of 3.25 days (1-30 days) between doses. Mean BK-HC grade decreased significantly by 1.8 (3.5 pre-cidofovir, 1.7 post-cidofovir, p<0.01). Overall, 66% of patients had response to cidofovir (CR=4, PR=4), with similar response rates between intravenous (66%) and intravesical (62%) administration. Two patients had reemergence of BK-HC after showing an initial response. Over the study period, 67% of patients died. Renal toxicity was experienced by 33% of patients; 3 patients had acute kidney injury (2 receiving intravesical, 1 receiving both modalities). Further complications included keratitis, Fanconi's syndrome, and pseudomonal sepsis after intravesical administration.
Discussion:
In our retrospective institutional review, a majority of patients achieved at least partial remission after cidofovir treatment with similar response rates between intravesical and intravenous administration. While the rate of CR was lower in our study (33%) than previous studies (60-100%), only severe BK-HC cases were included. Nonetheless, there was an overall significant reduction in BK-HC severity with cidofovir administration. While avoidance of systemic toxicity is a purported benefit of intravesical instillation, amongst patients receiving intravesical cidofovir, acute kidney injury as a possible complication needs to be considered. While cidofovir may be an efficacious therapy for BK-HC, albeit with potential demonstrated toxicities, further prospective trials are needed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal